Weighing the Benefits and Risks
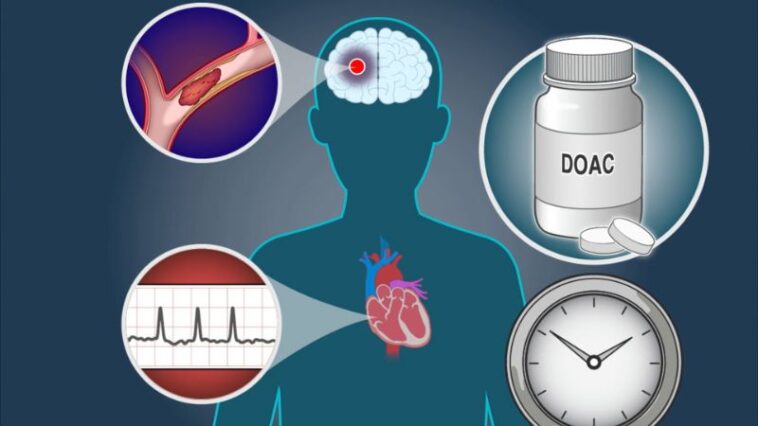
In the complex landscape of stroke management, the question of when to initiate anticoagulation therapy in patients with severe stroke and atrial fibrillation (AF) is a topic of intense debate. The early administration of anticoagulants can potentially prevent recurrent strokes but also carries significant risks, particularly hemorrhagic complications. Leading experts in neurology and cardiology have divergent views on this critical issue.
The Case for Early Anticoagulation
Proponents of early anticoagulation argue that the benefits outweigh the risks. Atrial fibrillation is a major risk factor for stroke recurrence, and anticoagulants are effective in reducing this risk. Dr. Sarah Thompson, a neurologist, highlights that “early anticoagulation can prevent the formation of new clots, which is crucial in the acute phase of stroke management.”
Recent studies suggest that early anticoagulation might reduce mortality rates and improve functional outcomes in selected patients. By preventing secondary strokes, patients have a better chance of recovery and rehabilitation. Moreover, modern anticoagulants, such as direct oral anticoagulants (DOACs), have a more predictable pharmacological profile and lower bleeding risks compared to traditional warfarin, making them a viable option in the early stages post-stroke.
The Argument Against Early Anticoagulation
On the other hand, opponents caution against the premature use of anticoagulants due to the high risk of hemorrhagic transformation. Dr. James Williams, a cardiologist, emphasizes that “the brain is particularly vulnerable after a severe stroke, and introducing anticoagulants too early can lead to devastating intracerebral hemorrhage.”
Clinical guidelines typically recommend a delay in anticoagulation initiation to allow for the stabilization of the infarcted brain tissue. This cautious approach aims to balance the prevention of recurrent ischemic events with the minimization of hemorrhagic complications. Studies have shown that the risk of hemorrhage is significantly higher in the first few days post-stroke, suggesting that a delayed approach may be safer for most patients.
Striking the Right Balance
The optimal timing for anticoagulation initiation in severe stroke patients with AF remains uncertain, with ongoing research and clinical trials seeking to provide more definitive answers. The decision must be individualized, taking into account the patient’s overall health, stroke severity, and bleeding risk.
Dr. Emily Roberts, a stroke specialist, summarizes the dilemma: “It’s a delicate balancing act. We need to weigh the potential benefits of early stroke prevention against the grave risk of hemorrhage. Multidisciplinary teams must work closely to tailor treatment plans for each patient.”
Conclusion
The debate over early anticoagulation in severe stroke patients with atrial fibrillation underscores the complexity of stroke management. While early anticoagulation may offer significant benefits in preventing recurrent strokes, the associated risks cannot be ignored. Ongoing research and clinical judgment will continue to shape best practices, aiming to improve outcomes for this vulnerable patient population. Early anticoagulation in severe stroke with AF: a delicate balance between risk and benefit.
Follow Wat-Not on Facebook, Twitter, and Instagram



GIPHY App Key not set. Please check settings